Scalp Acupuncture Points Pdf
- Zhu Scalp Acupuncture
- Scalp Acupuncture For Tremors
- Scalp Acupuncture Points Pdf Online
- Yamamoto New Scalp Acupuncture
- Scalp Acupuncture Points Pdf
- Scalp Acupuncture Map
Traditional medicine (TM) is increasingly accepted by people in the developing and developed world as an alternative to conventional treatments.14 One-third of American residents seek service from TM practitioners every year for illnesses that do not respond to conventional treatment.15 Acupuncture, which involves the insertion of fine needles into the skin at specific points, has a long history of use in China and is one of the important treatments used in TM. There are therefore two of these lines, one on each side of the head. 3) The Horizontal line on the back of the head at the level of the external occipital protuberance. 4) The Anterior Hair Line which is 3 cm above the eyebrows. The location of the 15 stimulation areas of scalp acupuncture and their therapeutic indications are as follows:. Yamamoto New Scalp Acupuncture (YNSA) was developed in Japan in 1973 by Toshikatsu Yamamoto. The method is based on a somatotope, in which the entire organism is projected on a defined area of the scalp. Here the focus lies on the Y-points, which represent meridians and which are located temporal. In 2006 a new point, the ZS-point(Zeise.
Abstract
Chinese scalp acupuncture is a contemporary acupuncture technique integrating traditional Chinese needling methods with Western medical knowledge of representative areas of the cerebral cortex. It has been proven to be a most effective technique for treating acute and chronic central nervous system disorders. Scalp acupuncture often produces remarkable results with just a few needles and usually brings about immediate improvement, sometimes taking only several seconds to a minute.
Each point is mapped out, listed by condition, point name is also listed by Chinese name with detailed description of point location. Acupuncture Point Locations - PDF 2.5 MB Detailed anatomical acupuncture point locations with cardinal points, command points and five element correspondences. Anatomy Charts - PDF Spinal anatomy, shoulder.
Acupuncture, a therapeutic technique of Oriental Medicine, can be traced back more than 2500 years. Throughout its long history, acupuncture has evolved as its own unique traditional medicine. By embracing newly developed knowledge and technology, the profession continues to create additional methods of treatment. Techniques such as electrical and laser acupuncture and even new acupuncture points are currently being developed. We believe scalp acupuncture, which integrates Western medicine with Traditional Chinese Medicine, to be the most significant development that Chinese acupuncture has made in the past 60 years.
INTRODUCTION
Chinese scalp acupuncture is a contemporary acupuncture technique integrating traditional Chinese needling methods with Western medical knowledge of representative areas of the cerebral cortex. It has been proven to be a most effective technique for treating acute and chronic central nervous system disorders. Scalp acupuncture often produces remarkable results with just a few needles and usually brings about immediate improvement, sometimes taking only several seconds to a minute.
HISTORY
Acupuncture, a therapeutic technique of Oriental Medicine, can be traced back more than 2500 years. Throughout its long history, acupuncture has evolved as its own unique traditional medicine. By embracing newly developed knowledge and technology, the profession continues to create additional methods of treatment. Techniques such as electrical and laser acupuncture and even new acupuncture points are currently being developed. We believe scalp acupuncture, which integrates Western medicine with Traditional Chinese Medicine, to be the most significant development that Chinese acupuncture has made in the past 60 years.
Scalp acupuncture is a well-researched natural science and incorporates extensive knowledge of both the past and present. Years of clinical experience have contributed to its recent discoveries and developments, but treatment of disorders by needling the scalp can also be traced back to early civilizations. In 100 BCE, the first Chinese acupuncture text, Huang Di Nei Jing (The Yellow Emperor's Classic of Internal Medicine) described the relationship between the brain and the body in physiology, pathology, and treatment as it was understood at that time, and citations of acupuncture treatments on the head can be found throughout classical Chinese literature.
The modern system of scalp acupuncture in China has been explored and developed since the 1950s. Various famous physicians introduced Western neurophysiology into the field of acupuncture and explored correlations between the brain and human body. In these early years of its development, there were several hypotheses for mapping stimulation areas. For example, Fan Yunpeng mapped the scalp area as a prone homunculus with the head toward the forehead and the legs toward the occipital area.1 Taking a dividing line that connects the left ear to the vertex to the right ear, Tang Song-yan proposed two homunculi on the scalp, one in prone position and another in supine position.2 Zhang Ming-jiu's and Yu Zhi-shun's scalp locations are formulated by penetrating regular head points, and Zhu Ming-qing created several special therapeutic bands on the scalp.3,4
It took acupuncture practitioners in China roughly 20 years before they accepted a central theory that incorporated brain functions into Chinese medicine principles. Dr. Jiao Shun-fa, a neurosurgeon in Shan Xi province, is the recognized founder of Chinese scalp acupuncture. He systematically undertook the scientific exploration and charting of scalp correspondences starting in 1971. Dr. Jiao combined a modern understanding of neuroanatomy and neurophysiology with traditional techniques of Chinese acupuncture to develop a radical new tool for affecting the functions of the central nervous system. Dr. Jiao's discovery was investigated, acknowledged, and formally recognized by the acupuncture profession in a national acupuncture textbook, Acupuncture and Moxibustion, in 1977.5 Ten years later, at the First International Acupuncture and Moxibustion Conference held in Beijing, China, scalp acupuncture began to gain international recognition. At the time, scalp acupuncture was primarily used to treat paralysis and aphasia due to stroke. Since then, the techniques and applications of this science have been expanded and standardized through further research and experience. Many studies on scalp acupuncture have shown positive results in treating various disorders of the central nervous system. The most outstanding results are with paralysis and pain management in very difficult neurological disorders.
CHARACTERISTICS
Scalp acupuncture, sometimes also called head acupuncture, is a modern innovation and development. Just like any new technology and science, the discovery, development, and clinical application of scalp acupuncture has undergone a period of challenge because it falls outside some fundamental theories of Chinese medicine as well as being a new concept in the Western world. As a contemporary acupuncture technique, many of the specific treatments put forward in this book are also new, at least for a work that discusses Western medical concepts along with Chinese ones.
Zhu Scalp Acupuncture
There are three new principles in this presentation of scalp acupuncture, however, which are of central importance and which depart considerably from traditional Chinese medicine. The first of these principles is the location of scalp acupuncture areas based on the reflex somatotopic system organized on the surface of the scalp in Western medicine. These do not relate to the theory of channels in Chinese medicine and are an essentially new type of conception. Second, because the technological innovation and invention of scalp acupuncture is fairly new, positive results can only reasonably be achieved by practitioners who have studied it; even an established doctor in China cannot perform it without at least seeing a demonstration of it. Third, scalp acupuncture consists of needling areas rather than points on the skull according to the brain's neuro-anatomy and neurophysiology. Unlike traditional acupuncture, where one needle is inserted into a single point, in scalp acupuncture needles are subcutaneously inserted into whole sections of various zones. These zones are the specific areas through which the functions of the central nervous system, endocrine system, and channels are transported to and from the surface of the scalp. From a Western perspective, these zones correspond to the cortical areas of the cerebrum and cerebellum responsible for central nervous system functions such as motor activity, sensory input, vision, speech, hearing, and balance.
In clinical practice, acupuncture treatments are typically based not just on a systematic or rigidly applied system, but also on highly individualized philosophical constructs and intuitive impressions. The practitioner has a wide amount of discretion on the use of points and techniques. Therefore, even when treating the same complaint, the method of treatment chosen by one practitioner can vary significantly from another. Scalp acupuncture, on the other hand, applies more of a Western medicine approach, where patients with the same diagnosis usually receive the same or very similar treatment.
The scalp somatotopic system seems to operate as a miniature transmitter-receiver in direct contact with the central nervous system and endocrine system. By stimulating those reflex areas, acupuncture can have direct effects on the cerebral cortex, cerebellum, thalamo-cortical circuits, thalamus, hypothalamus, and pineal body. The scalp's unique neurological and endocrinal composition makes it an ideal external stimulating field for internal activities of the brain. Scalp acupuncture treats and prevents disease through the proper insertion of needles into scalp areas. It is accompanied by special manipulations to regulate and harmonize the functional activities of the brain and body, as well as to restore and strengthen the functions of the body, organs, and tissues.
Scalp acupuncture successfully integrates the essence of ancient Chinese needling techniques with the essence of neurology in Western medicine. Studying its results in clinical practice can also add clarity to ambiguities found in the practice of neurophysiology and pathology. In terms of Western medicine, it contributes significantly to the treatment of central nervous system disorders. In complementary and alternative medicine, it contributes new understanding to both theory and practice. Scalp acupuncture can successfully treat many problems of the central nervous system such as paralysis and aphasia, for which Western medicine has little to offer.
APPLICATIONS
Scalp acupuncture areas are frequently used in the rehabilitation of paralysis due to stroke, multiple sclerosis, automobile accident, and Parkinson's disease. These areas may also be effectively employed for pain management, especially that caused by the central nervous system such as phantom pain, complex regional pain, and residual limb pain. It has been proven to have very effective results in treating aphasia, loss of balance, loss of hearing, dizziness and vertigo. The disorders covered in this book are commonly found in Western clinics. This book will show the scope of scalp acupuncture in treating many kinds of disorders and diseases, based on years of clinical experience. Scalp acupuncture not only treats disorders, but also can prevent illness and help to build the immune system. It can help increase energy, preserve youth, and promote longevity. The technique of scalp acupuncture is systematic, logical, easy to understand, and easy to practice. The techniques introduced in this book can be easily mastered and performed even by people with minimal acupuncture experience. Scalp acupuncture is more easily accessible, less expensive, entails less risk, can yield quicker responses, and causes fewer side effects than many Western treatments. Practitioners should consider scalp acupuncture as either the primary approach or a complementary approach when treating disorders of the central nervous system and endocrine system.
Although acupuncture and moxibustion have been used to prevent and treat disease in China for thousands of years, scalp acupuncture is a modern technique with a short history. In the West, many healthcare practitioners are familiar with acupuncture for pain management, while scalp acupuncture as a main tool for rehabilitation is a relatively new concept. It is still not easy for medical practitioners and the public to accept the reality that acupuncture can help in the recovery of paralysis, aphasia, and ataxia, while Western medical technology does not so far have effective treatments for those conditions. It is not surprising for a Western physician to claim that it is a coincidence if a patient recovers from paralysis after acupuncture. Therefore, there is an urgent need for Chinese scalp acupuncture to be studied and perfected, and extensive research done to fully explore its potential and utility. Chinese scalp acupuncture has been taught and used sparingly in the West and there are few books published on the subject. With such little information available, it has been almost impossible to apply this technique widely and with confidence. This book supplies all the needed information to practice scalp acupuncture.
In addition to more than 29 years of clinical practice of scalp acupuncture, we have taught scores of seminars for both practitioners of Chinese medicine and Western physicians practicing acupuncture in the USA and Europe, including eight years of seminars sponsored by UCLA and Stanford University. This book contains many amazing case reports from our years of clinical practice and teaching as examples of what is possible using these techniques. While it is not our intention to assert that scalp acupuncture is always effective with every patient, these clinical reports make a compelling case for its wider use. For example, in a report about the scalp acupuncture treatment of seven veterans with phantom limb pain at Walter Reed Army Medical Center in 2006, the results were as follows. After only one treatment per patient, three of the seven veterans instantly felt no further phantom pain, three others reported having very little pain, and only one patient showed no improvement. Such results warrant continued research into other possible uses for scalp acupuncture to alleviate human suffering.
During our lectures around the world, we are often asked why, if it is so effective in treating disorders of the central nervous system, has scalp acupuncture not spread to the whole world and been applied widely in practice? First, up to now there has been no authoritative and practical text for scalp acupuncture in English. Second, there is a very limited number of highly experienced teachers. Third, manual manipulation is very difficult to learn and master without detailed description and demonstration. And fourth, the names of stimulation areas are different from the standardized names given by the Standard International Acupuncture Nomenclature of the World Health Organization, Section 3.6 on Scalp Acupuncture, in Geneva in 1989.
Furthermore, there have been few reports or articles published on treatment by scalp acupuncture. Most existing textbooks either lack detailed information or only introduce some new research on the topic. From their teachers and textbooks, students can learn only general information about scalp acupuncture and its locations and clinical applications. Therefore, many practitioners in both the West and the East are only mildly aware of this new technique, and few apply it in their practices. There is a high demand for a book that can provide teachers and students with useful knowledge and offer proper references to experienced practitioners. We feel confident that this book will meet these requirements.
Part One of this book is designed to give practitioners fundamental knowledge of neuroanatomy, neurophysiology, and pathology in Western medicine. Chapter One provides a review for practitioners with a Western medical background and an adequate introduction for practitioners new to this material. The next chapter is a review of essential theories of Chinese medicine related to scalp acupuncture including the Four Seas theory and the Four Qi Street theory that provide readers with a systematic explanation of function and indication based on Chinese medicine. Chapter Three describes in detail locations and techniques of scalp acupuncture in order to offer a wide range of useful information for teachers, experienced or new practitioners, and students. Readers may notice that the indications for treatment for each scalp area are many in order to demonstrate the variety of disorders that can benefit from scalp acupuncture therapy. Finally, Chapter Four presents a large number of treatment strategies and techniques with color figures clearly illustrating the location of stimulation areas.
In Part Two of our book, we discuss in detail many common central nervous disorders. All of these have proven to respond well to scalp acupuncture treatment. Forty-five successful case histories are given from our clinical experience. In these case descriptions, we explain in practical detail how to apply the needling techniques in order to obtain optimal results. These cases demonstrate practical application of the principles of scalp acupuncture. Each one reflects our experience, thought processes, strategies, and special techniques for treating patients suffering from disorders of the central nervous system. Wherever possible or useful, other modalities or techniques to enhance the scalp acupuncture treatments are included with the case histories, which demonstrates the integration of Chinese medical theory and application into the clinical practice of scalp acupuncture. A few “miracle” cases are presented in this book, such as the woman who was completely cured of quadriplegia after only two scalp acupuncture treatments and a man who was cured of aphasia after just five. While more the exception than the rule, such cases demonstrate not only how remarkable these new techniques are, but also provide the readers with examples of real clinical practice using them.
The information presented in the book is primarily a synthesis of two components of knowledge of scalp acupuncture. First, we were among an early group of people who studied these techniques and were very fortunate to have opportunities to learn it directly from famous scalp acupuncture specialists including Jiao Shun-fa, the brilliant founder of Chinese scalp acupuncture, Yu Zhi-shun, a well-known professor in scalp acupuncture development, and Sun Shentian, an outstanding professor in scalp acupuncture research. Second, we have been teaching, practicing, and researching it for 29 years, both in China and in the US and Europe, and have accumulated extensive and valuable experience, which has given us insight into the needs and questions of acupuncture practitioners in Western clinical settings. Through this book, we hope to contribute this knowledge and experience to current and future students, practitioners, and teachers, and that it will serve as a stepping stone for further teaching, practice, research, and development of Chinese scalp acupuncture.
PART TWO
CHAPTER FIVE
Paralysis
Paralysis refers to complete or partial loss of muscle strength and voluntary movement for one or more muscles. Paralysis can be localized, generalized, or it may follow a certain pattern. Paralysis is most often caused by damage to the nervous system, especially the brain and spinal cord. Such damage may be due to stroke, trauma with nerve injury, poliomyelitis, amyotrophic lateral sclerosis, botulism, spinal bifida, and multiple sclerosis. Paralysis due to stroke, multiple sclerosis, and traumatic injury of the brain or spinal cord are the most commonly seen problems in our practice. Most paralyses caused by nervous system damage are constant in nature. There are forms of periodic paralysis, including sleep paralysis, which are caused by other factors. Paralysis can be accompanied by a loss of feeling in the affected area if there is sensory nerve damage as well.
The chain of nerve cells that runs from the brain through the spinal cord out to the muscles is called the motor pathway. Normal muscle function requires intact connections all along this motor pathway. Damage at any level often interrupts the brain's ability to control muscle movements resulting in paralysis. Paralysis almost always causes a change in muscle tone. Paralyzed muscles may be flaccid, flabby, and without appreciable tone, or may be spastic, tight, and with abnormally high tone that increases when the muscle is moved. Paralysis may affect an individual muscle but it usually affects an entire body region. The distribution of weakness is an important clue to locate the level of nerve damage that caused the paralysis.
The types of paralysis are classified by region. Monoplegia is impairment in the motor function of only one limb. Diplegia affects the same body region on both sides of the body (both arms, for example). Hemiplegia, affects one side of the body. Paraplegia is impairment in motor function of both legs and the trunk. Quadriplegia, also known as tetraplegia, is paralysis with partial or total loss of use of all limbs and the torso. Paralysis is also divided into four types in neurological practice, namely upper motor neuron paralysis, lower motor neuron paralysis, paralysis due to neuromuscular transmission diseases, and the paralysis caused by muscular diseases.
To test the strength of each muscle group and record it in a systematic fashion is important before and after scalp acupuncture treatment for paralyzed patients. It can help localize a lesion to a particular cortical region and spinal cord level, evaluate scalp acupuncture treatment, and give the patient encouragement when there is subtle improvement that the patient might not notice. When evaluating a patient with paralysis, the practitioner should follow a systematic approach that includes inspection of muscle, palpation and percussion of muscle, manual muscle strength testing, and assessment of motor function. It is useful to pair the testing of each muscle group immediately with the testing of its contra-lateral counterpart to enhance detection of any asymmetries and record detailed information of any changes.
| • monoplegia is impairment in the motor function of only one limb |
| • diplegia affects the same body region on both sides of the body (both arms, for example) |
| • hemiplegia affects one side of the body |
| • paraplegia is impairment in motor function of both legs and the trunk |
| • quadriplegia, also known as tetraplegia, is paralysis with partial or total loss of use of all limbs and the torso |
Muscle strength is often rated at six levels on a scale of 0 out of 5 to 5 out of 5.6,a The level of 0 out of 5 shows no muscular contraction, which means complete paralysis; the level of 1 out of 5 shows some muscular contraction, but no limb or body movement; the level of 2 out of 5 shows limb movement is possible but not against gravity, which means the limb can only move in its horizontal plane; the level of 3 out of 5 shows limb movement is possible against gravity but not against resistance by the examiner; the level of 4 out of 5 shows limb movement is possible against some resistance by the examiner but it is still weak compared to a normal limb; and the level of 5 out of 5 shows normal muscular strength, which means complete recovery from paralysis.
Scalp acupuncture is frequently used in rehabilitation of paralysis due to stroke, multiple sclerosis, spinal cord injury, and traumatic brain injury. It has been proven effective in treating any type of paralysis, sometimes taking only one to two treatments for an amazing amount of recovery. We have treated hundreds of paralyzed patients with remarkable results in the US, China, and Europe, allowing many patients to leave their wheel-chairs, walkers, crutches, and canes behind.7–
Since scalp acupuncture is a modern technique with just 39 years of history, much more research needs to be done so that its potential can be fully explored and utilized and more paralyzed patients helped to regain a normal life.
STROKE
Stroke is an acute neurological disease in which the blood supply to the brain is interrupted causing brain cells to die or be seriously damaged, thus impairing brain functions. Stroke is classified into two major categories, ischemic and hemorrhagic. In an ischemic stroke, a blood vessel becomes occluded and the blood supply to part of the brain is blocked. Ischemic stroke is divided into thrombosis stroke, embolic stroke, systemic hypoperfusion, and venous thrombosis. A hemorrhagic stroke occurs when a blood vessel in the brain ruptures and bleeds. The bleeding vessel can no longer carry the blood to its target tissue and interrupts the brain's blood supply. Hemorrhagic stroke is commonly divided into two types, intracerebral and subarachnoid.
The symptoms of stroke depend on the type of stroke and the area of the brain affected. These include weakness, paralysis or abnormal sensations in limbs or face, aphasia, apraxia, altered vision, problems with hearing, taste, or smell, vertigo, disequilibrium, altered coordination, difficulty swallowing, and mental and emotional changes. Some stroke patients may have loss of consciousness, headache, and vomiting at the onset. If the symptoms disappear within several minutes up to a maximum of 24 hours, the diagnosis is transient ischemic attack (TIA), which is a mini or brief stroke. Those symptoms are warning signs and a large proportion of patients with TIA may develop full strokes in the future.
Stroke is the third leading cause of death in the United States after heart attack and cancer and it is a leading cause of adult disability. It is necessary for stroke patients to receive emergency treatment with Western medicine and it is important to identify a stroke as early as possible because patients who are treated earlier are more likely to survive and become less disabled. Stroke survivors usually have some degree of sequelae of symptoms depending primarily on the location in the brain involved and the amount of brain tissue damaged. Disability affects about 75% of stroke survivors and it can affect patients physically, mentally, emotionally, or a combination of all three.
Because each side of the brain controls the opposite side of the body, a stroke affecting one side of the brain results in neurological symptoms on the other side of the body. For example, if stroke occurs in the motor area of the right side of the brain, the left side of the body may show weakness or paralysis. Although there is no cure for stroke, most stroke patients now have a good chance for survival and recovery. When stroke patients pass the acute stage they should start rehabilitation as soon as possible. Stroke rehabilitation therapy helps patients return to normal life as much as possible by regaining and relearning skills of everyday living such as speaking or walking. Treatment may include acupuncture, physical therapy, occupational therapy, speech and language therapy, and massage.
In Chinese medicine, the stroke itself is thought to involve several interpromoting disease mechanisms, possibly including qi stagnation, heat, phlegm, blood stasis and, of course, wind. Hence the common name for stroke in Chinese medicine is wind stroke. Many of these same patterns will be present in cases involving post-stroke symptomology discussed in this book such as paralysis, dysphagia, and aphasia.
CASE HISTORY #1
At a workshop conducted at Tri-State Acupuncture College in New York City in 1998, a patient named Tom volunteered for scalp acupuncture. The manager at the college told us that the patient had had a stroke from cerebral thrombosis only 11 months before and was a good candidate for the class demonstration. While interviewing Tom, we were shocked to find that his right arm and hand had actually been paralyzed for 11 years. Although we were not at all certain that we could help this patient, it had taken several hours for the family member to give him a ride here and we did not want to turn him away. His tongue was a little purple with a normal coating and his pulses were bilaterally fine and wiry.
As an additional source of concern, we had only a few hours earlier told the students that any patient with paralysis enduring for more than three years was unlikely to respond to scalp acupuncture therapy. Unsure how to proceed, we considered simply demonstrating the location and technique of scalp acupuncture on this patient and not immediately showing the results to the students. After demonstrating two needles in his scalp, we moved Tom to another room to rest, inserted more needles, and then continued with the lecture.
Chinese medical pattern discrimination: Qi stagnation and blood stasis in the channels and network vessels
SCALP ACUPUNCTURE TREATMENT
Area selection
Primary area: Upper 1/5 and middle 2/5 of the Motor Area Secondary area: Upper 1/5 and middle 2/5 of the Sensory Area
Manipulation
For treating motor dysfunction, place the needles and rotate them at least 200 revolutions per minute for 1–3 minutes every 10 minutes for a total of 30–60 minutes. The worse the symptoms or longer the duration of disease, the longer the duration of each treatment should be. As stated above in Chapter Four, unless the paralysis is due to the removal of damaged tissue by brain surgery, a paralyzed extremity is generally treated by choosing the opposite side of the Motor Area on the scalp. The upper 1/5 region is used to treat contralateral dysfunctional movement of the lower extremity, trunk, spinal cord, and neck. The doctor should twirl the needle as vigorously as the patient can tolerate and have the patient move the affected limb actively and passively. It is helpful to have the patient exercise the affected limbs with or without assistance as indicated, between needle stimulations.13 During treatment, some patients may have sensations of heat, cold, tingling, numbness, heaviness, distention, or the sensation of water or electricity moving along their affected limbs. Those patients usually respond and show improvement quickly. However, those who don't have such sensations could still have immediate effects. Initially, treatment should be two to three times a week until major improvements are achieved, then once weekly, then every two weeks, and then spaced out as indicated by the patient's condition. A therapeutic course consists of 10 treatments.
RESULTS OF CASE #1
Tom was instructed to do some passive exercise while the needles were in place, having his wife move his hand and raise his arm. While we were continuing our lecture, we heard screaming from the other room. The patient's wife rushed back into the lecture room saying repeatedly, “He can move his arm and hand now” in a loud, excited voice. Tom was able to move his arm, hand, and even his fingers in any way or direction that he was asked by the audience. This patient's experience has caused us to change the information we give students about whether treatment could be successful after a specific number of years. It is now our opinion that a patient with paralysis should be treated no matter how long ago a stroke has occurred as long as the limb shows no muscular atrophy. One student at this class offered the conclusion, “It's never too late to treat a paralyzed patient with scalp acupuncture.”
DISCUSSION
Scalp acupuncture has been found to have very good effects on the sequelae of stroke including hemiplegia, aphasia, and abnormal sensations in the limbs. Thanks to advanced stroke research and brain imaging technology, doctors are continuing to gain new understanding of how the brain can adapt after stroke in order to regain its ability to function. New research suggests that normal brain cells are highly adaptable. They can undergo changes not only in function and shape but also can take over the functions of nearby damaged cells. Because of these abilities, scalp acupuncture is geared toward stimulating and restoring affected brain tissue or retraining unaffected brain tissue to compensate for the lost functions of damaged brain tissue.
In Tom's case, the hemiplegia was caused by cerebral thrombosis, which has the best prognosis for recovery from stroke compared to cerebral embolism and cerebral hemorrhage. It is necessary to point out, however, how unusual it is that a patient gets only one scalp acupuncture treatment and recovers completely. In our normal practice it often takes from several weeks to several months for stroke patients to improve and recover.
Also, the time frame for patients with stroke to be treated by scalp acupuncture is crucial; the earlier the treatment the better the prognosis. When treating stroke from thrombosis or embolism, scalp acupuncture treatment should begin as soon as feasible. When treating a hemorrhagic stroke, however, scalp acupuncture should not be performed until the patient's condition is stable, probably one month after a stroke.
As we discovered with Tom, a patient with any duration of stroke disabilities can be treated, but treatment within a year brings about the greatest response in our experience. The longer the duration of the impairment, the more gradual will be the improvement. With long-term conditions expectations need to be realistic, although occasionally a patient will surprise practitioners. It is hardest to achieve improvement for a patient with paralysis for a long time, especially if there is also muscular atrophy and rigid, inflexible joints.
There are several different acupuncture techniques to treat paralysis. Although scalp acupuncture has the best and fastest response, other techniques are necessary for a fuller recovery. According to the individual's condition, regular body acupuncture, electrical acupuncture, and moxibustion, as well as physical therapy and massage can combine with scalp acupuncture to speed up the time of recovery. Regular acupuncture treatment has been found to have positive therapeutic effects on the recovery of movement in the hands, fingers, feet, and toes. In treating unilateral paralysis of the limbs, traditionally more points from yang ming channels are selected because yang corresponds to movement and agility, and foot yang ming stomach channel controls muscle functions. Commonly used points are He Gu (LI 4), Wai Guan (TB 5), Qu Chi (LI 11), Bi Nao (LI 14), and Jian Yu (LI 15) for upper limb paralysis, and Kun Lun (Bl 60), Cheng Shan (Bl 57), Yang Ling Quan (GB 34), Zu San Li (St 36), and Huan Tiao (GB 30) for lower limb paralysis. Although more yang ming points are used for paralysis, points from yin channels, especially tai yin and jue yin channels should not be ignored. Yin corresponds to nourishing muscles and tendons and points from yin channels have positive results for pronounced stiffness and contraction of the limbs. Commonly used points are Chi Ze (Lu 5) and Nei Guan (Per 6) for upper limbs and San Yin Jiao (Sp 6), Yin Ling Quan (Sp 9), Xue Hai (Sp 10), and Qu Quan (Liv 8) for lower limbs. Hand or foot paralysis is relatively difficult to recover and often requires a longer process, especially for a contracted hand and foot. To relax contractures of the hand, thread a two-inch needle from He Gu (LI 4) under the palm toward Lao Gong (Per 8) and Hou Xi (SI 3). Stimulate this needle with vigorous thrusting, lifting, and twirling. Thread another needle deeply from Wai Guan (TB 5) toward Nei Guan (Per 6) and stimulate in a similar fashion. To relax the upper arm and shoulder, thread a needle from Jian Yu (LI 15) to Bi Nao (LI 14) and stimulate vigorously. To relax contractures of the foot and ankle, thread a two-inch needle from Jie Xi (St 41) toward Qiu Xu (GB 40) and Sheng Mai (Bl 62). Thread a second needle from Jie Xi (St 41) toward Zhong Feng (Liv 4) and Zhao Hai (Ki 6). Thread a third needle from Tai Chong (Liv 3) through the foot to Yong Quan (Ki 1) on the sole of the foot. Stimulate all needles with vigorous thrusting, lifting, and twirling. For additional effect, thread a long needle from Yang Ling Quan (GB 34) through to Yin Ling Quan (Sp 9) and from Kun Lun (Bl 60) through to Tai Xi (Ki 3).
Electrical stimulation is very helpful if the practitioner has difficulty performing needle rotation of more than 200 times per minute. It is suggested that only one to two pairs of the scalp needles be stimulated at any one session or the brain can become too confused to respond. For electrical stimulation in body acupuncture, fewer than four needles should be stimulated in each limb. Best results are achieved by applying low frequency (for example, 3 hertz) with high intensity (for instance, when visible muscle contraction is observed). Moxibustion can enhance the therapeutic results of scalp acupuncture, especially for older or weaker patients.
Research on the effect of scalp acupuncture for stroke
There are considerable clinical studies and experimental research showing the excellent results obtained from scalp acupuncture on paralysis due to stroke.
Jiao Shun-fa, the founder of scalp acupuncture, collected and analyzed 20,923 cases of paralysis caused by stroke from 1970 to 1992. After treatment on the Motor Area of the scalp, 7,637 cases were cured (36.5%), 7,117 cases showed marked improvement (34%), and 5,196 cases showed some improvement (24.8%), yielding a total effective rate of 95.13%.14
Jia Huai-yu reported on 1,800 cases of paralysis due to stroke treated on the Motor Area by scalp acupuncture in 1992. The result were as follows: 462 cases fully recovered (25.67%), 950 cases markedly improved (52.78%), 292 cases somewhat improved (16.22%), 96 cases failure (5.33%), yielding a total effective rate of 94.67%. Findings in these two studies are very similar.15
Liu Jian-hao and colleagues reported on the treatment of 60 cases of paralysis due to stroke using scalp acupuncture in 2010. The duration of the paralysis was from one day to 14 days. The patients were randomly divided into a body acupuncture group and a scalp acupuncture group, 30 in each group. The body acupuncture group was treated with needling from Bai Hui (GV 20) penetrating to Tai Yang (extra point) and the scalp acupuncture group was treated at the Motor Area. Treatments were given once a day and 14 treatments comprised a course. The neurological deficit scores (NDS) and the therapeutic effects were compared before and after treatment and the contents of plasma endothelins (ET) and calcitonin gene related peptide (CGRP) were tested on the second and four-teenth days respectively after initial treatment. The results showed that the effective rate was 86.7% (26/30) in the body acupuncture group and 80.0% (24/30) in the scalp acupuncture group. The NDS of both groups were statistically decreased (P < 0.01). The ET level was also decreased and the CGRP level was effectively increased in both groups (P< 0.01).
DYSPHAGIA
Dysphagia is the medical term for the symptom of difficulty in swallowing. The signs and symptoms of dysphagia include difficulty controlling food in the mouth, inability to control food or saliva in the mouth, difficulty initiating a swallow, coughing, choking, frequent pneumonia, unexplained weight loss, gurgly or wet voice after swallowing, nasal regurgitation, and swallowing difficulty. When asked where the food is getting stuck, patients will often point to the cervical region. The actual site of obstruction is always at or below the level at which patients perceive the obstruction. The most common symptom of esophageal dysphagia is the inability to swallow solid food, which the patient often describes as “becoming stuck” or “held up” before it either passes into the stomach or is regurgitated. Some people present with “silent aspiration” and do not cough or show outward signs of aspiration. When the airway is unprotected and foreign material is aspirated into the lungs, the person is at risk for development of pulmonary infection and aspiration pneumonia. A swallowing disorder can occur in people of all age groups but it is more likely in the elderly, patients who have had strokes, and in patients who are admitted to acute care hospitals or chronic care facilities.
Dysphagia is classified into two major types, oropharyngeal dysphagia and esophageal dysphagia. Oropharyngeal dysphagia is often caused by stroke, multiple sclerosis, myasthenia gravis, Parkinson's disease, amyotrophic lateral sclerosis, and Bell's palsy. Esophageal dysphagia can be subdivided into mechanical and functional causes. Functional causes include achalasia, myasthenia gravis, and bulbar or pseudobulbar palsy. Mechanical causes usually comprise peptic esophagitis, carcinoma of the esophagus or gastric cardia, candida esophagitis, and pharyngeal pouch. Medicines can help some people, while others may need surgery. Treatment with a speech-language pathologist can help. Patients may find it helpful to change their diet or hold their heads or necks in a certain way when they eat. In very serious cases, patients may need feeding tubes.
CASE HISTORY #2
Fred, a 62-year-old male in a wheelchair, was brought to our clinic in Santa Fe, NM. His wife gave a brief medical history because of his aphasia. One month before, Fred had severe headache, slurred speech, and the right side of his body became paralyzed. A local hospital diagnosed stroke caused by cerebral hemorrhage in his left hemisphere. He initially was totally paralyzed on the right side and had lost his speech. He had been receiving physical therapy and speech therapy since he was admitted to the hospital. Although his aphasia gradually improved, his speech was not clear. His voice was low and it was very difficult to understand him. He had severe dysphagia and could not swallow any food or water at all, which was his primary complaint at our clinic. He felt depressed, irritable, angry, and severely fatigued. A nasogastric tube was inserted to provide non-oral feeding. Examination showed he was unable to move his right leg and foot at all with muscular tone at 0 out of 5. He could move his right arm slightly with muscular tone at 2 out of 5. He could not elevate the hyoid bone, indicating a probable swallow reflex problem. Maximum phonation duration of seven seconds indicated reduced breath support, likely resulting from vocal cord paralysis. He had a weak cough and diminished throat-clearing ability. His aphasia, dysphasia, and paralysis on the right side had shown no further improvement for the past two weeks. A hospital physician recommended that Fred try acupuncture treatment. Upon examination he looked very tired and depressed, his tongue was red with a dry, thick, yellow coating, and his pulses were wiry and slippery.b
Chinese medical pattern discrimination: Liver depression qi stagnation, spleen qi deficiency, blood stasis in the channels, liver-gallbladder damp heat
SCALP ACUPUNCTURE TREATMENT
Area selection
Primary area: Upper 1/5, middle 2/5 and lower 2/5 Motor Area
Secondary area: Speech I Area (same as lower 2/5 Motor Area), Neck point, (a new extra point for dysphagia, located at 1 inch below Feng Chi (GB 20)
Manipulation
The entire Motor Area should be needled and stimulated on the opposite side of the paralyzed limbs. Always put one needle in the ear point Shen Men to help a depressed and angry patient relax and to reduce the sensitivity of needle insertion and stimulation of the scalp. Use the fewest number of needles possible in the scalp and rotate the needles at least 200 times per minute with the thumb and index finger for 2–3 minutes, twirling as gently as possible so that the depressed patient can tolerate the sensation and repeating the stimulation every 10 minutes. Select the Speech I Area or some local points in the neck accordingly if the patient has aphasia or difficulty swallowing. Retain the needles in place for 30–45 minutes. The treatment is given two to three times per week and a therapeutic course consists of 10 treatments. Communicate with the patient and any relatives often in order to gain their confidence, to encourage them, and reduce their fear and anxiety.
During the treatment, some patients may experience sensations of heat, cold, tingling, numbness, heaviness, distention, or the sensation of water or electricity moving along their spine, legs, or arms. Telling the patient that those are normal and that people who experience some or all of these sensations usually respond and improve more quickly encourages them to come back for additional treatments. However, those who do not have such sensations could still have immediate positive results.
RESULTS OF CASE #2
Fred was very negative and showed no interest in treatment by scalp acupuncture at the initial visit. He was reluctant to do any active exercise when being instructed. Even after showing some improvement of his aphasia and the paralyzed arm and leg, he demonstrated no excitement and simply said, “I do not notice any difference about my throat and swallowing.”
At the second treatment, Fred presented with severe depression and no motivation. He did not like to perform speech, swallowing, and body exercises. His treatment strategy was modified to take care of depression. The ear points Heart, Liver, and Shen Men along with the Head Area and Chest Area on the scalp were needled.
At the beginning of the third visit, his wife reported that Fred's mood and attitude were much better after the last treatment. He talked a little more and was easier to understand. To her surprise he reminded her what time he had the acupuncture appointment that day. Since the patient's attitude was relatively more positive toward acupuncture therapy, we were able to perform stronger stimulation after inserting needles at the same locations as for the initial treatment. Fred was able to follow instructions to practice his speech and do oral and pharyngeal exercises. He started to smile after hearing himself count from one to 10 very clearly. He refused to try drinking a little bit of water to test his swallowing function and said he was afraid that it could induce severe coughing and choking and cause aspiration. With continued encouragement Fred finally agreed to try. To his astonishment he did not choke at all when he took a first sip of water. He drank more and more and finished a whole cup of water without a problem.
The patient thrived on this program. He began to tolerate a soft/semi-solid diet and the nasogastric feeding was gradually tapered down to overnight only as his oral intake improved. At this point his weight increased and his stamina was markedly improved. Fred started to eat more solid food and add more kinds of food gradually.
With every treatment, Fred showed dramatic improvements in speech, eating and drinking, and movement of his right arm, hand, leg, and foot. By the fifth treatment, Fred wanted to add more foods and soon could eat and drink anything like a normal person. The nasogastric tube was removed and he had no problem with talking or depression after his sixth treatment.
His subsequent treatments were focused on his paralyzed arm and leg. He was treated by combined scalp acupuncture and body acupuncture. For body acupuncture, Qu Chi (LI 11), Wai Guan (TB 5), and He Gu (LI 4) on the right upper limb and Zu San Li (St 36), Kun Lun (Bl 60), and Jie Xi (St 41) on the right lower limb were needled. Sometimes those points were stimulated with electrical acupuncture. Fred could move his right arm up and down more and he was able to start walking to our clinic on his own. After the sixteenth treatment he had gained more mobility and use of his right hand and gained more muscular strength in that hand. At the end of 20 treatments his walking appeared almost normal. At his last visit, Fred said, “Thank you very much for giving me back my normal life.”
DISCUSSION
Scalp acupuncture offers great rehabilitation tools for dysphagia. Most patients with dysphagia whom we have treated showed some improvement after three treatments and some of them appear better right way. However, to treat dysphagia patients who have depression is very challenging because patients are not always willing to participate in the treatment. It requires very good needle technique as well as good communication skills. Sometimes it is necessary to treat the depression first and then address the difficulty in swallowing. Compared to other patients, in general depressed patients should receive fewer needles, milder stimulation, and a shorter time of needle retention. Whether you are treating a child or adult with depression, it is important to observe the response and reaction while inserting, stimulating, or withdrawing needles, and adjust the techniques accordingly. Although each part of the cerebral cortex has its own functions, some variation is possible. When one area is impaired, this area can recover to a certain extent or can be compensated somewhat by other areas with proper scalp stimulation. This may be the mechanism by which scalp acupuncture is successful in treating dysphagia.
Correct food consistency, texture, and temperature are important for the dysphagia patient's success during acupuncture treatment. All three factors are important as they act to heighten lingual control, reduce oral muscle fatigue, minimize the patient's fear of choking, and provide a cohesive bolus to stimulate a swallow reflex. A dysphagia diet uses foods that stimulate swallowing and minimize mucus build-up around the larynx. Dysphagia may lead to malnutrition and dehydration and at the most severe stages can cause choking, aspiration, and airway obstruction. Therefore it is imperative to deal with the dangers of dysphagia through dietary management once acupuncture has been instituted. Overall, our patient Fred had a very successful recovery, progressing from dysphagia to total normal eating within just a few weeks. This case study followed the patient as his post-stroke swallowing status changed and various acupuncture decisions were made. In addition to scalp acupuncture, the ear and body acupuncture were very helpful in the patient's progress and recovery. This case illustrates that scalp acupuncture could be the primary approach to manage swallowing disorder.
Research on the effect of scalp acupuncture for dysphagia
Li Min and colleagues reported the treatment of 60 cases of dysphagia due to stroke using scalp acupuncture in 2009. The duration of the condition was from 30–360 days. The 60 cases were randomly divided into a five-needle-in-nape (FNN) group and a routine acupuncture (RA) group, 30 cases in each group. The FNN group was treated with needling Ya Men (GV 15), Tian Zhu (Bl 10), and Zhi Qiang Xue (new extra point). The RA group was treated with needling at Lian Quan (CV 23), Tong Li (Ht 5) and Zhao Hai (Ki 6). Treatment was given six times a week and 16 treatments made a course. Results showed seven cases fully recovered, 13 cases markedly improved, eight cases some improvement and two cases failure in FNN group. Five cases fully recovered, eight cases markedly improved, 11 cases some improvement, and six cases failure in the RA group. The effective rate was 93.3% in the FNN group, better than that of 80.8% in RA group (P< 0.05).
MULTIPLE SCLEROSIS
Multiple sclerosis (MS) is a progressive disease of the central nervous system in which communication between the brain and other parts of the body is disrupted. Its effects can range from relatively benign in most cases, to somewhat disabling, to devastating for some people. During an MS attack, inflammation occurs in areas of the white matter of the central nervous system in random patches. These are called plaques. This is followed by the destruction of myelin. Myelin allows for the smooth, high-speed transmission of electrochemical messages between the brain, the spinal cord, and the rest of the body. When myelin is damaged, neurological transmission of messages may be slowed or blocked completely resulting in some body functions being diminished or lost. Approximately 300,000 people in the US and 2.5 million people worldwide suffer from MS. It primarily affects adults, with age of onset typically between 20 and 40 years, and is twice as common in women compared to men.
Symptoms and signs of multiple sclerosis vary widely depending on the location of affected myelin sheaths. Common symptoms include numbness, tingling or weakness in one or more limbs, partial or complete loss of vision, double or blurred vision, tremor, unsteady gait, fatigue, cognitive impairment, and dizziness. Some patients may also develop muscle stiffness or spasticity, paralysis, slurred speech, dysfunction of urine or bowels, and depression. In the worst cases, people with MS may be unable to write, speak, or walk. Multiple sclerosis is unpredictable and varies in severity. In some patients it is a mild disease but it can lead to permanent disability in others. Multiple sclerosis may occur either in discrete attacks or slowly over time. Although symptoms may resolve completely between the episodes, permanent neurological problems usually persist, especially as the disease progresses.18 Many risk factors for multiple sclerosis have been identified, but no definitive cause has been found. It likely occurs as a result of some combination of environmental and genetic factors. Currently, multiple sclerosis does not have a cure in terms of conventional treatments. However, a number of therapies including acupuncture can be used to treat the disease symptomatically and convert MS into remission.
In Chinese medicine, there are at least six or more patterns of disharmony that can account for the signs and symptoms of multiple sclerosis. The common denominators in most cases are external invasion or internal engenderment of damp heat, which damages qi and consumes yin and blood, thus giving rise to internal stirring of wind. Former heaven or prenatal natural endowment insufficiency may also play a role.
CASE HISTORY #3
Denise, a 79-year-old female in a wheelchair, was brought to our clinic in Santa Fe, New Mexico, in 1994. She had suffered from multiple sclerosis for more than 25 years. Her initial symptoms were an onset of numbness in the right arm followed by subsequent numbness descending down both her legs. Over the past 25 years, Denise had multiple relapses and remissions with episodes of lower extremity weakness, stiffness and muscle spasm, incontinence of urine, loss of balance, and fatigue. Those symptoms typically lasted a few weeks to several months. Five years ago she had a dramatic neurological decline during which she was unable to stand up and lost strength and sensation in her lower extremities. For the last three years and currently, she could not stand or walk by herself due to weakness in her legs and loss of balance. Denise also complained of numbness, tingling, and spasms in her legs accompanied by incontinence of urine and severe fatigue. The examination revealed she had paraparesis of the left lower extremity that was more affected than the right. Her tongue was purple with a thin white coating. Her pulses were wiry and fine overall, with especially weak pulses in the cubit (chi) positions bilaterally.
Chinese medical pattern discrimination: Liver blood deficiency with internal stirring of liver wind, kidney qi deficiency, liver depression qi stagnation, blood stasis
SCALP ACUPUNCTURE TREATMENT
Area selection
Primary area: Motor Area, Sensory Area, Foot Motor and Sensory Area
Secondary area: Balance Area, Chorea and Tremor Area, and Vertigo and Hearing Area
Manipulation
Insert needles in the Motor Area, Sensory Area, and Foot Motor and Sensory Area and stimulate unilaterally or bilaterally according to the patient's symptoms. Rotate the needles at least 200 times per minute with the thumb and index finger for 1–3 minutes, twirling them as vigorously as the patient can tolerate and repeating the stimulation every 10 minutes. During treatment, some patients may have all or some of the following sensations: increasing tingling or numbness, heat, cold, heaviness, distention, or the sensation of water or electricity moving along their spine, legs or arms. Patients with some or all of these sensations usually respond and improve more quickly. However, those who do not have such sensations could still have immediate positive results. If balance, dizziness, or vertigo is present, select the Balance Area or the Vertigo and Hearing Area. The Chorea and Tremor Area should be chosen if the patient has tremor or limb spasms. Keep the needles in for 25–30 minutes. Treatment is given two to three times per week and a therapeutic course consists of 10 treatments.
RESULTS OF CASE #3
Denise had a very positive response to her initial scalp acupuncture treatment. She was amazed to feel the spasms and numbness in her legs improve just minutes after a few needles were inserted. Although she was nervous when the doctor asked her to stand up, her family was thrilled to see her not only stand up with improved stability, but also start to walk a few steps. At the second treatment, Denise reported that the incontinence of urine had improved remarkably after the first treatment and the numbness, spasms, and weakness of both legs showed some improvement as well. She continued to get better with each additional treatment and by the sixth treatment, Denise was able to enter our clinic with a walker instead of in a wheelchair. She also had more energy and started to do some housework again.
By the fifteenth treatment, Denise reported that she was able to walk around her home by herself and walk much longer distances. The numbness and tingling in her limbs did not bother her as much, she had more energy, and had not experienced incontinence of urine for several weeks. However, her right foot was still weak and was sometimes difficult to pick up and she had to drag it to walk. During each treatment, however, her right foot was getting stronger and she could pick it up more easily. This ability would last for several days after treatment, so Denise liked to get a tune-up treatment every other week. At each session, a few needles would be inserted in her scalp and she would go out for a walk and come back later for withdrawal of the needles.
DISCUSSION
When compared to other acupuncture modalities including acupuncture on the ear, body, and hand, scalp acupuncture has proven to have the most success in treating MS and other central nervous system damage. Not only can it improve symptoms, the patient's quality of life, and slow the progression of physical disability, but it can also reduce the number of relapses. The patient should get treatment as soon as possible as the earlier the treatment, the better the prognosis. Scalp acupuncture treatment for MS has had much success in reducing numbness and pain, decreasing spasms, improving weakness and paralysis of limbs, and improving balance. Many patients also have reported that their bladder and bowel control, fatigue, and overall sense of well-being significantly improved after treatment.
Recent studies have shown that scalp acupuncture can be a very effective modality in controlling MS, often producing remarkable results after just a few needles are inserted. It usually relieves symptoms immediately and may take only a few minutes to achieve significant improvement. Although scalp acupuncture areas may be chosen according to the patient's particular symptoms, primary areas for patients with motor problems such as paralysis, weakness of limbs, or abnormal sensations in limbs including tingling, numbness, or pain, are the Motor Area and the Sensory and Foot Motor Areas. Those areas should be stimulated unilaterally or bilaterally, according to the patient's manifestations. Select the Balance Area or Vertigo and Hearing Area of the scalp, respectively, depending on the symptoms. The Chorea and Tremor Area should be chosen if patients have limb spasm. Many patients have a very quick and positive response in controlling urine and bowel functions when the Foot Motor and Sensory Area is stimulated.
There are many different acupuncture techniques for treating MS. Although scalp acupuncture has the fastest track record for improving symptoms, other techniques are also necessary for further improvement. Regular body acupuncture, electrical acupuncture, and moxibustion as well as physical therapy and massage can be combined with scalp acupuncture to speed up recovery. Regular acupuncture treatment has been found to have a positive therapeutic effect on the recovery of movement and reducing abnormal sensations of the hands, fingers, feet and toes. Commonly used points are Feng Chi (GB 20), Yu Zhen (Bl 9), Nao Kong (GB 19), Huan Tiao (GB 30), Yang Ling Quan (GB 34), Tai Chong (Liv 3), and Tai Xi (Ki 3) for lower limbs, and Qu Chi (LI 11), He Gu (LI 4), and Wai Guan (TB 5) for upper limbs.19 Electrical stimulation is very helpful if the practitioner has difficulty performing needle rotation more than 200 times per minute. It is suggested that no more than two of the scalp needles be stimulated at any session so the brain does not become too confused to respond. Moxibustion can enhance the therapeutic results of scalp acupuncture, especially for older or weak patients. Recommended points are Zu San Li (St 36), San Yin Jiao (Sp 6), Guan Yuan (CV 4), Yong Quan (Ki 1) and Shen Shu (Bl 23).
When treating chronic progressive diseases like multiple sclerosis, Parkinsonism, and amyotrophic lateral sclerosis (ALS), the effects are sometimes temporary. Improvement may last for hours, days, weeks, or months, but follow-up treatments will be necessary on an ongoing basis. When treating paralysis, whether from stroke or trauma, improvements in movement are often permanent. The practitioner should consider scalp acupuncture as the primary approach rather than as a complementary approach for the patient with multiple sclerosis. Although other acupuncture techniques can be effective, scalp acupuncture seems to bring about quicker and often immediate improvement. In a recent investigation, scalp acupuncture was applied to 16 patients with multiple sclerosis at our National Healthcare Center in Albuquerque, NM. After only one treatment per patient, eight of the 16 patients instantly showed significant improvement, six patients showed some improvement, and only two patients showed no improvement, thus yielding a total effective rate of 87%.
CASE HISTORY #4
Michael, a 52-year-old patient referred by his primary care physician, walked with the aid of a cane. He sought treatment from us during a conference in Phoenix, Arizona, in 2006. He had suffered from multiple sclerosis since 1982 and had received many kinds of treatments with no positive results. Five years before, his medical team had noted his condition “has been slowly going downhill.” Because his legs were very stiff and weak, Michael had to drag both legs in a shuffling manner when he walked. Other symptoms included an inability to lift his feet or wiggle his toes. His fatigue was so great he could only walk 2–3 minutes at a time. Further examination showed that he could not stand with stability due to losing his balance when standing on both legs, and it was impossible for him to stand on one leg. He could neither utilize a normal gait from heel to toe nor walk backwards. His tongue was red and slightly purple with a thick, white coating and his pulses were wiry and slippery.
Chinese medical pattern discrimination: Spleen qi and kidney essence deficiency, liver depression with depressive heat leading to the internal stirring of liver wind
RESULTS OF CASE #4
While needles were being inserted in Michael's scalp the audience was quiet, waiting to see how he would respond to his first treatment. Michael showed remarkable improvement right away. When told that it was time for him to “show off,” he stood up straight with great stability and even stood on one leg for several seconds without losing his balance. The audience reported that he was taking much larger steps, was lifting up his legs rather than dragging them, and was turning around without hesitation. During the break, Michael went outside for a bit more exercise. He walked back into the conference room without using his cane and his face glowed with pleasure as he told the audience, “I walked for about 30 minutes without any rest and without my cane except for security. I am so overjoyed with these unexpected wonderful results. I can walk solidly from heel to toe and walk backwards with no difficulty.”
DISCUSSION
Although multiple sclerosis (MS) remains an incurable disease of the central nervous system, scalp acupuncture provides an important complementary/alternative treatment approach for improving many symptoms and the patient's quality of life by slowing or reversing the progression of physical disability and reducing the number of relapses. By directly stimulating affected areas of the central nervous system, scalp acupuncture has shown more effective results compared to other acupuncture techniques. Our studies showed that 87% of patients had instant improvement after only one treatment. Scalp acupuncture for MS is accessible, less expensive, safer, more effective, and causes fewer side effects than Western medical treatments. It not only benefits MS patients, but also significantly helps us to better understand the mechanisms that cause the condition. It may lead to the discovery of new effective treatments and hopefully to a cure for this disease in the future.
SPINAL CORD INJURY
Often caused by a car or sporting accident, spinal cord injury is extremely serious. When cervical discs are injured, compression fractures may cause permanent disability. Also hernias or bulges of intervertebral discs may cause spinal cord compression. Common symptoms of spinal injuries include arm and leg paralysis or weakness, difficulty breathing, tingling, numbness, or pain in affected limbs, and incontinence of both bowel and urine.
Modern medicine has not yet found a cure for spinal cord injury. The majority of treatments available in Western medicine involve drugs or surgery and are often ineffective. Acupuncture treats the patient as a whole entity and helps patients with spinal cord injury to recover function more effectively than Western medical treatment. If the spinal cord injury is not total, it is possible for some people to recover all bodily functions including touch and pain sensations, bladder and bowel functions, and motor control. Through acupuncture treatment, some patients can be cured and many others witness a variety of significant improvements.
CASE HISTORY #5
Julia, a 49-year-old female in a wheelchair, was brought to our clinic in Santa Fe, NM, in 1992. Four months prior to the first visit, this patient was injured in a car accident. Her neck was severely damaged at the level of C-5 and C-6. Upon examination, it was found that she had paralysis of all four extremities. Below the level of injury on the neck there was minimal contraction and movement of arm muscles, which indicated that the muscular tone of her arm was a 2 out of 5. Her hand, legs, and feet were completely paralyzed, which meant that muscular tones were 0 out of 5. Julia had incontinence of urine and was experiencing muscle spasms throughout her entire body. Her tongue was purplish with a thin, sticky, yellow coating. The pulse reading showed lack of force in the inch (cun) and bar (guan) positions, with faint pulses in the cubit (chi) position.
Chinese medical pattern discrimination: Qi stagnation and blood stasis in the channels, kidney qi deficiency
SCALP ACUPUNCTURE TREATMENT
Area selection
Primary area: Upper 1/5 Motor Area and middle 2/5 Motor Area
Secondary area: Foot Motor and Sensory Area, Chorea and Tremor Area
Manipulation
Needles should be inserted in both upper 1/5 Motor Area and middle 2/5 Motor Area and stimulated bilaterally. Rotate the needles at least 200 times per minute with the thumb and index finger for 1–3 minutes, twirling them as vigorously as the patient can tolerate and repeating the stimulation every 10 minutes. During the treatment, some patients may experience sensations of heat, cold, tingling, numbness, heaviness, distention, or the sensation of water or electricity moving along their spine, legs, or arms. Patients with some or all of these sensations usually respond and improve more quickly. However, those who do not have such sensations could still have immediate, positive results. Select the Chorea and Tremor Area or Foot Motor and Sensory Area according to whether the patient has muscular spasms or other abnormal sensations such as pain or burning. Retain the needles for 25–30 minutes. Treatment is given two to three times per week and a therapeutic course consists of 10 treatments.
RESULTS OF CASE #5
During the first treatment, Julia experienced immediate relief from the muscle spasms. She also experienced a sensation like electricity shooting downward through her spine, radiating to her feet. With more stimulation of the needles on her head, she started to feel a hot sensation in her hands and feet. She felt so excited about these improvements that she began to cry. While Julia was starting to wiggle her paralyzed toes, we told her that her responses were a good prognosis for significant improvement in the near future. During the third treatment she was able to stand on her feet with someone holding her knees and could lift her arms much higher. The incontinence of urine also showed some improvement. After each treatment from the third to the fifth visit there were gradual improvements in all her limbs.
During the sixth treatment, Julia was able to kick her legs with some strength and she could bend her legs at the knee and hold this position for a few minutes. This was a signal that she could possibly stand and walk. With strong encouragement, she struggled up and stood by herself for one minute, two minutes, and then three minutes. After resting for a while, she stood up again and started to walk, managing 20 halting steps before needing to sit down, exhausted. Julia was also in much better control of urination, now holding her urine for six hours at night. After the eighth treatment she was able to walk with the assistance of a walker, experienced much more mobility in her hand movements, and her body spasms were almost entirely gone. With the increase in hand functions she was able to hold a knife with both hands and cut vegetables. To be able to cook again brought her such tremendous joy and gratitude that she laughed and cried at the same time.
Though she continued to improve with each treatment, the most dramatic changes occurred in the twentieth treatment. At that time her leg and arm muscles were so much stronger that she was able to write and make phone calls. She called the Western medicine physician who had told her she would be paralyzed for the rest of her life and gave him the wonderful news. Not believing that she was once again able to walk, he went to her house in person to see this miraculous change. Though shocked and stunned watching her walk up to greet him, her doctor was thrilled with her progress and hoped for more excellent results. After 39 treatments, she had gained back all movement of her hands and arms, was able to walk with a cane, and began living without the aid of personal assistants. After 48 treatments, Julia felt well enough to end treatment and start a new life in San Francisco where her son was living.
DISCUSSION
Scalp acupuncture is the best therapy for spinal cord injury. Having proven effective through clinical results recorded over the last 35 years, it can effectively stimulate the paralyzed area in order to restore the body's energy flow to a normal state so that the body can heal itself. In other words, scalp acupuncture is able to treat the cause and thus heal the injury. It is also the most useful technique for the patient to improve quickly in the initial visits. In our practice, the combination of scalp acupuncture and regular body acupuncture ensures the best results, especially for the further recovery of paralyzed fingers and toes. Common acupuncture points include Qu Chi (LI 11), He Gu (LI 4), Jian Yu (LI 15), and Wai Guan (TB 5) for upper limb paralysis and Yang Ling Quan (GB 34), Huan Tiao (GB 30), Feng Shi (GB 31), Zu San Li (St 36), and Kun Lun (Bl 60) for lower limb paralysis. Electrical acupuncture is very helpful for speeding up recovery and can be applied on the above points as well as at the Hua Tou Jia Ji points on the back. When choosing Hua Tou Jia Ji points, the pair of points for stimulation should be one above and one below the site of injury level. The electrical stimulation usually lasts 10–20 minutes. Exercise is very important for the recovery of affected limbs. Regular exercise helps the blood circulation and keeps muscles active, and this also accelerates the results from ongoing acupuncture treatments.
Scalp Acupuncture For Tremors
TRAUMATIC BRAIN INJURY
Traumatic brain injury is a serious condition that may lead to permanent or temporary impairment of the brain's functions. Brain damage is often related to quick acceleration and deceleration of the brain, which results in injury to the area of impact and its opposite area. The symptoms of brain injury depend on the area of the brain affected. When the speech and motor areas are damaged, body dysfunctions appear such as aphasia and paralysis.
According to Chinese medicine, trauma to the head (or anywhere else in the body) causes the blood to extravasate outside its normal vessels, obstructing the flow of fresh new blood to the area. Any tissue of the body requires nourishment by blood to perform its proper function. Blood stasis must be resolved for the tissue to once again receive the nourishment of healthy blood.
CASE HISTORY #6
Lisa, a 10-year-old girl in a wheelchair, was brought by her mother to our clinic in Santa Fe, New Mexico, in 1993. Four months before, Lisa fell off her bicycle and hit her head on the left side, above and behind her ear. She had had a concussion on the left side of the brain in the internal capsule and initially was totally paralyzed on her right side and lost the ability to speak. She had been receiving rehabilitation treatment including physical therapy, osteopathic therapy, and speech therapy starting two weeks after her injury. Her aphasia gradually improved and she was able to drag her right leg while walking and move her right arm slightly but the paralysis had shown no further improvement for the past eight weeks. Her primary doctor recommended that she try acupuncture treatment. Upon examination, her tongue was red with a thin white coating and her pulse was slippery and wiry.
Chinese medical pattern discrimination: Qi stagnation and blood stasis in the channels
SCALP ACUPUNCTURE TREATMENT
Area selection
Primary area: Upper 1/5 Motor Area and middle 2/5 Motor Area
Secondary area: Foot Motor and Sensory Area, Chorea and Tremor Area
Manipulation
Needles should be inserted in both upper 1/5 Motor Area and middle 2/5 Motor Area and stimulated on the opposite side of the paralyzed limbs. With children, select the thinnest needles that you can insert into the scalp. Always put one needle in the ear point Shen Men to help a young patient relax and to reduce the sensitivity of needle insertion and stimulation of the scalp. Use the fewest number of needles possible in the scalp and rotate them at least 200 times per minute with the thumb and index finger for one minute, twirling as gently as possible so that the child patient can tolerate the sensation and repeating the stimulation every 10 minutes. Communicate with children and their parents more often than with adult patients in order to reduce their fear and anxiety. During the treatment, some patients may experience sensations of heat, cold, tingling, numbness, heaviness, distention, or the sensation of water or electricity moving along their spine, legs, or arms. Tell the child that those are normal and are a good sign for improving more quickly.
Select the Chorea and Tremor Area or Foot Motor and Sensory Area according to whether the patient has muscular spasms or other abnormal sensations such as pain or burning. Retain the needles in place for 10–20 minutes.
Treatment is given two to three times per week and a therapeutic course consists of 10 treatments.
RESULTS OF CASE #6
Lisa was afraid of needles and started to cry and refuse the treatment before the first needle was inserted. She agreed to allow the needle insertion only after her mother told her that she might ride a bike again if these treatments worked. The insertion of two needles on the left side of her scalp did not seem to bother her at all. Two minutes after the treatment began, Lisa announced that she felt “a lot of blood move to my head.” After that, the child was able to lift her right arm with much more ease. Her walking also showed some improvement as she was able to lift her right leg more easily.
Lisa experienced dramatic improvements of her right arm, hand, leg, and foot with every visit. By the sixth treatment, Lisa could move her right arm up and down very quickly and was able to start writing with that hand again. After the fifteenth treatment, she had gained more mobility and use of her right hand as well as more muscle strength in that hand, which was now as strong as her left hand. Her walking appeared almost normal, and she was again able to run, at least slowly. At the end of the twenty-second treatment her right hand was completely back to normal and all paralysis was gone. She had participated in running a race and did very well.
DISCUSSION
Scalp acupuncture can be an excellent rehabilitation tool for traumatic brain injury patients. However, while treating children with body acupuncture can be challenging, it can be even harder with scalp acupuncture. Children and their parents might not be willing to participate in needling as a therapeutic method. It requires the doctor to have very good techniques of insertion and manipulation of needles as well as good communication skills. Sometimes it is necessary to show a patient how tiny the needles are or demonstrate the insertion of a needle in the practitioner's own body. This helps to reduce fear and anxiety for both patient and parents.
It is very helpful to play or chat with young patients as if they are friends or family members before the treatment. It is also a good strategy to ask the parents to talk, play with, or feed young patients during the insertion and stimulation of needles, which acts as a diversion to turn the child's attention away from the needles and makes them less sensitive to the procedure. For a child who is extremely sensitive to needles, stimulation by twirling should be avoided during the first one or two visits. For children less than two years old, an effective technique is to hide each needle from their sight while inserting and stimulating. Compared to adult patients, generally speaking, young patients should receive fewer needles, milder stimulation, and shorter time of needle retention. Whether you are treating a child or adult, it is important to observe responses and reactions while inserting, stimulating, or withdrawing needles, and adjust the techniques accordingly.
CASE HISTORY #7
David, a 52-year-old man, was vacationing with his wife in Santa Fe, NM, in 1993. A waitress who noticed that he was paralyzed told him that he should come to our clinic, which specialized in treating that affliction. The man had developed paralysis in the right arm and hand after an operation on the left side of his brain to remove a tumor. Following the surgery, the left front side of his head no longer contained any scalp and there was a depression where the tumor and surrounding tissue had been removed. Because he was feeling very frustrated with his condition, David took the advice of the waitress and made an appointment at our clinic for a free consultation the same day. In addition to the paralysis on the right side, his tongue was purple with teeth marks and a thin, white coating. His pulses were wiry and fine.
Chinese medical pattern discrimination: Qi stagnation and blood stasis in the channels
SCALP ACUPUNCTURE TREATMENT
Area selection
Primary area: Upper 1/5 Motor Area and middle 2/5 Motor Area
Manipulation
Needles should be inserted in the upper 1/5 Motor Area and the middle 2/5 Motor Area on the unaffected side of the scalp for patients who develop paralysis from brain surgery. Always put one needle in the ear point Shen Men to help nervous patients relax and reduce the sensitivity of needle insertion and stimulation of the scalp. Rotate the needles at least 200 times per minute with the thumb and index finger for 1–3 minutes, twirling them as vigorously as the patient can tolerate and repeat the stimulation every 10 minutes. During treatment, some patients may experience sensations of heat, cold, tingling, numbness, heaviness, distention, or the sensation of water or electricity moving along their spine, legs, or arms. As mentioned previously, those patients with some or all of these sensations usually respond and improve more quickly. One may also choose the Chorea and Tremor Area or Foot Motor and Sensory Area accordingly if the patient has muscular spasms there. Retain the needles for 25–30 minutes. Treatment is given two to three times per week and a therapeutic course consists of 10 treatments.
RESULTS OF CASE #7
During the initial consultation, David and his wife asked many questions because they were doubtful that scalp acupuncture could help him. They asked, “How quickly could he notice any improvement?” David decided to try the treatment but was still skeptical after being told that some patients had immediate improvement and others did not. Examination showed that the sensations in his right arm and hand were still normal. There was a little twitching in the muscles of his arm but no movement at all in his right arm or hand and the hand appeared puffy and swollen.
After two needles were inserted on the right side of his scalp, David immediately noticed tingling sensations in his right arm and hand. A few minutes later he was able to move his paralyzed arm and hand, amazed as he raised it over his head. The following day he returned to the clinic for another treatment. David appeared to be very tired because, he said, “Everyone at the hotel came to our room for hours to shake my recovering hand.” By the end of his fifth treatment David had full use of his right hand and arm and the edema in his hand was completely gone.
BELL'S PALSY
Bell's palsy is a paralysis and weakness of the muscles that control expression on one side of the face. The disorder results from damage or trauma to one of a pair of facial nerves (Cranial Nerve VII) that controls the muscles of the face. Symptoms of Bell's palsy usually appear suddenly and reach their peak within 48 hours. Symptoms range in severity from mild weakness to total paralysis of the face, and Bell's palsy can often cause significant facial distortion. Until recently, in most cases its cause was unknown. Most scientists believe that a viral infection causes the disorder and that the facial nerve swells and becomes inflamed in reaction to the infection.
Signs and symptoms of Bell's palsy may include sudden onset of weakness or paralysis on one side of the face making it difficult to smile or close the eye on the affected side, and deviation and droop of the corner of the mouth making facial expressions difficult. Other symptoms include pain behind or in front of the ear on the affected side, sounds that seem louder on the affected side, and changes in the amount of tears and saliva the body produces. Babies can be born with facial palsy and they exhibit many of the same symptoms as adults with Bell's palsy. This is often due to a traumatic birth that causes irreparable damage to the facial nerve resulting in acute facial nerve paralysis.
Patients with facial paralysis for which an underlying cause can be readily found are not generally considered to have Bell's palsy. These underlying problems include tumor, stroke, diabetes, meningitis, head trauma, and inflammatory diseases of the cranial nerves. However, the neurological findings are rarely restricted to the facial nerve in these conditions. There is no cure or specific treatment for Bell's palsy, although three in four patients' symptoms may subside on their own within two to three weeks. Others may be left with deficits of varying degrees, and some patients have permanent damage.
Major complications of the condition include chronic loss of taste (ageusia), chronic facial spasm, and corneal infections. To treat loss of taste, the lower 2/5 Sensory Area in the scalp should be stimulated. It is not advisable to use electrical stimulation on the needles in the face because it may cause facial muscle spasm. To treat facial muscle spasm the Chorea and Tremor Area and the lower 2/5 Motor Area should be stimulated. To prevent corneal infections, the eyes may be protected by covers or taped shut during sleep and for rest periods. Tear-like eyedrops or eye ointments may be recommended, especially in cases of complete paralysis.
Facial paralysis, according to Chinese medicine, involves both disregulation of qi and blood causing mal-nourishment of the channels in the facial region, as well as invasion by pathogenic wind-cold or phlegm.
CASE HISTORY #8
Jimmy, a 52-year-old male, came to our clinic in Santa Fe, NM, in 2000. He had been diagnosed with Bell's palsy two weeks prior and was suffering from cold-like symptoms. He was experiencing moderate pain running along the line of his jaw and behind his left ear. As well, he could not close his left eye, raise his left eyebrow, show his upper teeth, frown, or puff out his left cheek. If this was not enough, the corner of his mouth on the affected side drooped and his mouth deviated to the right side, which was aggravated when he smiled. Because of all these symptoms, he was extremely agitated, angry, and fearful that his face would never look normal again. He had a red tongue with a thin, yellow coating. His pulses were wiry and slippery.
Chinese medical pattern discrimination: Damp heat obstructing the channels and network vessels
SCALP ACUPUNCTURE TREATMENT
Area selection
Primary area: Lower 2/5 Motor Area
Secondary area: Lower 2/5 Sensory Area
Manipulation
Needles should be inserted on both lower 2/5 Motor Area and lower 2/5 Sensory Area on the contralateral side. Select the finest gauge needles that you can insert into the scalp for the initial treatments. Always put one needle in the ear point Shen Men to help the patient relax and reduce sensitivity to needle insertion and stimulation of the scalp. For two minutes, rotate the needles at least 200 times per minute with the thumb and index finger, twirling them as gently as possible at the beginning of treatment and repeating stimulation every 10 minutes so that the patient can tolerate the sensations better. During treatment, some patients may have all or some of the following sensations: heat, cold, tingling, numbness, heaviness, distention, or the sensation of water or electricity moving in the affected side of the face. Retain the needles in place for 20–30 minutes and request the patient to exercise the affected side of his facial muscles during scalp acupuncture treatments, especially if there are no needles in his face. The treatment is first given two times per week and then gradually reduced to fewer sessions after patients have experienced major improvement. A therapeutic course consists of 10 treatments.
RESULTS OF CASE #8
Jimmy had a very good response to his first scalp acupuncture treatment. He was immediately able to close his left eye better and the pain around his ear and jaw significantly reduced just a few minutes after two needles were inserted. After the third treatment, the deviation and drooped corner of his mouth showed remarkable improvement, especially after more needles were inserted into his face, hands, and feet. He was able to raise his left eyebrow, reveal his upper teeth, and puff out his left cheek after only six visits. However, he still could not squeeze his left eye completely closed and his smile was a little crooked. After nine scalp acupuncture treatments, he regained all functions of expression in his face and was very pleased with the outcome.
DISCUSSION
Scalp acupuncture is an effective treatment for Bell's palsy. It can repair damaged nerves and restore full use and strength to injured areas. Most patients can recover completely after five to 15 treatments. The sooner patients get treatment, the quicker their recovery. However, facial paralysis may continue to develop and get worse for seven to 10 days after initial symptoms occur.
If treating a patient with Bell's palsy within seven days of its onset, it is wise to inform patients that their condition is not yet stable and more or worse symptoms can continue to develop. Otherwise, patients may conclude that acupuncture made their symptoms worse. Although scalp acupuncture has been successful in the treatment of Bell's palsy, body acupuncture with threaded techniques is very effective for this disorder as well. Common points are Si Bai (St 2) threaded toward Di Cang (St 4), Di Cang (St 4) threaded toward Jia Che (St 6), Yu Yao (extra point) threaded toward Tai Yang (extra point), Yang Bai (GB 14) threaded toward Yu Yao (extra point), and Xia Guan (St 7), He Gu (LI 4), and Tai Chong (Liv 3).
Research on the effects of scalp acupuncture for Bell's palsy
There are several clinical studies showing the excellent results obtained from scalp acupuncture and regular body acupuncture on facial paralysis.
Wu Jian-min reported on treating 80 cases of facial paralysis using scalp acupuncture in 1989. The duration of the ailment was from four days to two years. Scalp acupuncture treatments were given once a day and 10 treatments made a course. The results showed Bell's palsy fully resolved in 72 cases (90%) and markedly improved in 8 cases (10%) with zero failure, yielding an effective rate of 100%.20
Based on Liu Fang-shi's report of research done in 1994, 48 cases of facial paralysis were treated by scalp acupuncture on the Motor Area. The results were 25 cases fully recovered (52%), 18 cases markedly improved (38%), and 5 cases failed to improve at all (10%), yielding a total effective rate of 90%.21
MOTOR NEURON DISEASES
The motor neuron diseases (MNDs) refer to a group of progressive neurological disorders that affect motor neurons associated with controlling voluntary muscle activity including speaking, walking, breathing, swallowing, and general movement of the body. They commonly have distinctive differences in their origin and causation but a similar result in their outcome for the patient, which is severe muscle weakness. Common MNDs include amyotrophic lateral sclerosis (ALS), primary lateral sclerosis, progressive muscular atrophy, and poliomyelitis. Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig's disease, is a disorder that generally involves either the lower or upper motor systems of the body. In advanced stages, both regions of the body are affected. It is caused by sclerosis in the corticospinal tracts.
Primary lateral sclerosis is a rare motor neuron disease that resembles ALS but there is no evidence of the degeneration of spinal motor neurons or muscle wasting that occurs in ALS.
Progressive muscular atrophies are a wide group of genetic disorders characterized by primary degeneration of the anterior horn cells of the spinal cord, resulting in progressive muscle weakness.
Poliomyelitis, also called polio or infantile paralysis, is a highly infectious viral disease that may attack the central nervous system and is characterized by symptoms that range from a mild nonparalytic infection to total paralysis. Common symptoms and signs include progressive weakness, muscle wasting, muscle fasciculations, spasticity or stiffness in the arms and legs, and overactive tendon reflexes. Patients may present dragging foot, unilateral muscle wasting in one or the other hand, or slurred speech.
Causes of many motor neuron diseases are unknown and others have varying causes according to the specific motor neuron disease. There is no cure or standard treatment for motor neuron diseases and treatment focuses on reducing the symptoms of muscle spasm and pain while maintaining the highest practical level of overall health.
Diseases such as progressive muscular atrophy, poliomyelitis, and ALS are categorized as wei zheng () or wilting conditions in Chinese medicine. The patterns presenting in these diseases usually include a complex combination of liver blood, kidney yin, and spleen qi deficiencies along with damp heat further consuming the blood and damaging the qi, and thus depriving the limbs of strength and the flesh and muscles of nourishment. The damp heat may become congested in the network vessels causing the sinews and muscles to further lose their nourishment. Other patterns based on the patient's constitutional tendencies may also present or arise as the disease progresses.
CASE HISTORY #9
Sherry, a 38-year-old female, came to our clinic in 2007. It was difficult for her to walk even with her mother's support and because of Sherry's aphasia, her mother gave the medical history. Sherry fell frequently, lost her balance easily, and had had difficulty walking since the age of 19. Her slurred speech sometimes even her mother could not understand. She could not control her urine, choked when eating, and always felt fatigued. Her left ovary hurt and the pain was worse during menses. She often had a migraine headache and premenstrual syndrome (PMS), and she had considerable mucous in her nose and throat much of the time. Sherry had been to several famous hospitals but there was no clear diagnosis. Several doctors thought she suffered from a motor neuron disorder or ALS. Her mental activity presented as normal and she was then in graduate school for a master's degree.
Examination showed she was unable to stand and walk straight by herself. Her gait was wide-based and unsteady and she had to hold on to someone to walk in order to maintain her balance. Her ataxia was even more apparent when she tried to turn and her whole body was stiff and rigid, but worse on the left side. She had lost her fine motor skills. Her legs had severe tremors when she put her toes on the ground and she could not stand on one leg. She counted the numbers from one to 20 with a slow, slurred, weak voice. She could hardly be understood when she said her home phone number. Her tongue had a red tip, a peeled coating on the right side, was purple in the center, had major teeth marks along the sides, a severe tremor, and a thick, white coating. Her pulses were fine and wiry, and were faint in both cubit (chi) positions.
Chinese medical pattern discrimination: Liver wind stirring internally, kidney qi deficiency
SCALP ACUPUNCTURE TREATMENT
Area selection
Primary area: Upper 1/5 Motor Area and Speech I Area
Secondary area: Foot Motor and Sensory Area, Chorea and Tremor Area, and Praxis Area
Manipulation
Insert needles in the upper 1/5 Motor Area, Speech I Area, Foot Motor and Sensory Area, Chorea and Tremor Area, and Praxis Area and stimulate bilaterally. Rotate the needles at least 200 times per minute with the thumb and index finger for 1–3 minutes, twirling them as vigorously as the patient can tolerate and having the patient move her affected limbs actively and passively. Repeat the stimulation every 10 minutes. During treatment, some patients experience sensations of heat, cold, tingling, numbness, heaviness, distention, or the sensation of water or electricity moving in the affected limbs. Those patients usually respond and improve more quickly. However, those who don't have such sensations could still experience immediate and positive effects. Retain the needles for 30–45 minutes and treat two or three times a week. A therapeutic course consists of 10 treatments.
RESULTS OF CASE #9
A few minutes after being needled on her head, Sherry felt a whole-body hot sensation, which then moved from her hips to her feet, stronger on the left side. Afterwards, her speech was so much clearer, faster, and stronger that even she was surprised. Her walking was much more stable and she was able to lift both legs much higher. She could stand on either leg alone and had to look down to check if it was true.
She returned for the second treatment a day later, having had traveled across the country for these treatments. Sherry reported without her mother's help that her body was less stiff and that she could walk and move better. Her speech was clearer, she didn't feel that her tongue was thick when talking, and very little choking had occurred. Her fatigue and bladder control were improved but she still had a lot of mucous and leg tremor. Her bowel movements were a little loose and she had experienced some nausea and gas after taking the prescribed Chinese herbs. Examination showed that the tremor as well as teeth marks in her tongue were less, the thick, white coating was less, and it was peeled more on the front part of her tongue. Her pulses remained unchanged.
During the second treatment, Sherry experienced a hot sensation again, more so on the left side of the body. She was able to count from one to 20 without breathing. She felt that her legs were not as heavy when walking. For scalp acupuncture, the Chorea and Tremor Area replaced the Foot Motor and Sensory Area in this second treatment. Body acupuncture was added 15 minutes after scalp acupuncture began. The points were Tai Chong (Liv 3), Tai Xi (Ki 3), Yang Ling Quan (GB 34), Feng Long (St 40), Wai Guan (TB 5), and Lian Quan (CV 23).
During the third treatment the next day, the patient reported that she walked better with more control of her left leg and that it felt less heavy. Her speech continued improving with less of a heavy sensation in her tongue. She was able to eat better because of less choking. She had less mucous in her nose and throat and no nausea since the last visit. Although the tremor in both legs was better, she still had some fine movement problems such as difficulty with buttons and writing and still had some stiffness in her legs. Examination showed that her tongue was less red with fewer teeth marks and tremor only on the left side. The thick, white coating was less. Her pulses remained unchanged and were still fine and wiry.
The treatment strategy was modified. While the same scalp areas of upper 1/5 Motor Area and Speech I Area were still used, the Praxis Area and Chorea and Tremor Area were added to address her secondary complaints. The manipulation and retaining of needles remained the same. She could pick up pennies on a table with either hand during the treatment.
Two days later, Sherry arrived for her fourth session and reported very positive reactions to the last treatment. Eating was easier because she could swallow without choking and had less mucous in the throat. Her breathing was less labored when she was active, and friends noticed major improvement in her speech during phone conversations. Sherry's fine motor movement showed some improvement such as turning on a light switch. Unfortunately, that morning she had lost her balance and fallen backward, but with no severe injury. Her tongue showed a red tip, only a thin, white coating, and a peeling coating at the front. There were almost no teeth marks remaining. Her fine pulses had become a little larger and stronger, were still slightly wiry, and showed more strength in the cubit (chi) positions.
Ayyappan song download. Nov 17, 2018 Download Ayyapan Songs Malayalam, Tamil, Telugu, Kannada, Ayyappan Songs latest collections,ayyappan songs,ayyappan songs download,ayyappan songs mp3. May 02, 2018 Click on the “Download MP3” link to download the file Chord Lagu Ayyappan Hit Song Dowland Mp4. All the MP3 files are downloaded directly from Youtube CDN server.
She received more aggressive treatment that day because it was her last treatment for this trip. The upper 1/5 Motor Area and Speech I Area were still considered primary according to her condition. The Speech III Area, Balance Area, and Foot Motor and Sensory Area were added to assist and consolidate her improved clinical signs. She responded immediately after the needles were inserted, her voice sounding much clearer and stronger. She reported that her balance was improving and her legs felt lighter during the walking exercises. She watched and listened to herself on the video screen while she walked and talked like a normal person. At the end of her final treatment she was both laughing and crying.
DISCUSSION
Scalp acupuncture has been found to have very a significant positive impact on hemiplegic aphasia due to various central nerve disorders, even during the initial few treatments. In Sherry's case, the hemiplegia was caused by a motor neuron disorder. For patients such as Sherry who present with multiple symptoms and signs, it is, in our experience, more effective to treat major complaints first with a few needles. Secondary symptoms can be addressed after patients have significant improvements in their major complaints. As the above case study demonstrated, doctors should modify the treatment strategy and stimulate areas according to changes in a patient's condition.
In our practice, the combination of scalp acupuncture and regular body acupuncture ensures the best results, especially for the further recovery of paralyzed fingers or toes. Common acupuncture points include He Gu (LI 4), Qu Chi (LI 11), Jian Yu (LI 15), and Wai Guan (TB 5) for upper limb paralysis and Yang Ling Quan (GB 34), Feng Shi (GB 31), Huan Tiao (GB 30) Zu San Li (St 36), and Kun Lun (Bl 60) for lower limb paralysis. Electrical acupuncture is very helpful for speeding up recovery. The electrical stimulation usually lasts 10 to 20 minutes. Exercise is also important for the recovery of affected limbs. Active and passive exercise during scalp acupuncture treatment is very important for improvement. It helps the blood circulation and keeps muscles active, accelerating the results from ongoing acupuncture treatments.
QUADRIPLEGIA
Quadriplegia means paralysis of all four limbs or of the entire body below the neck. When the arms, legs, and torso are paralyzed, this is commonly caused by damage to the brain, injury of the cervical spinal cord, polyneuritis, myasthenia gravis, progressive myodystrophy, multiple myositis, or acute infective multiple radiculoneuritis.
The severity of quadriplegia depends on both the level at which the spinal cord is injured and the extent of the injury. Although the most obvious symptom is impairment to the limbs, function is also impaired in the torso. That results in loss or impairment of bowel and bladder control, sexual function, digestion, breathing, and other autonomic functions. Because sensation is usually impaired in affected areas, this can manifest as numbness, reduced sensation, or burning sensation and pain. Quadriplegics are often vulnerable to pressure sores, osteoporosis and fractures, frozen joints, spasticity, respiratory complications and infections, poor autonomic reflexes, deep vein thrombosis, and cardiovascular disease because of depressed functioning and immobility.
CASE HISTORY #10
Barbara was in a wheelchair when she was brought to our 2006 scalp acupuncture seminar in Phoenix, Arizona. She had little hope that our treatment would help her condition. Infected by West Nile virus, she had immediately developed quadriplegia. She lost control of her body below the neck and had paralysis of all four limbs. As a result, she had incontinence of bowel and urine. After trying many kinds of therapies that brought no improvement, she became depressed. Examination showed that all four extremities were very tight and had occasional spasms. The muscular tone of her right arm ranked 2 out of 5 degrees, and her left arm and both legs were 0 out of 5 degrees, or completely paralyzed. Her tongue was red with a thin, white coating; her pulses were fine and wiry.
Chinese medical pattern discrimination: Qi stagnation and blood stasis in the channels, kidney qi deficiency, liver blood deficiency and liver depression qi stagnation
SCALP ACUPUNCTURE TREATMENT
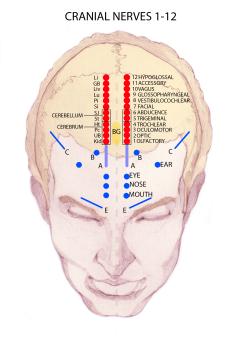
Area selection
Primary area: Upper 1/5 and middle 2/5 of Motor Area
Secondary area: Foot Motor and Sensory Area
Manipulation
Needles should be inserted in both upper 1/5 Motor Area and middle 2/5 Motor Area and stimulated bilaterally. Rotate the needles at least 200 times per minute with the thumb and index finger for 1–3 minutes, twirling them as vigorously as the patient can tolerate and repeating the stimulation every 10 minutes. During treatment, some patients feel heat, cold, tingling, numbness, heaviness, distention, and/or the sensation of water or electricity moving along their spine, legs, or arms. Patients who experience some or all of these sensations usually respond and improve more quickly. As stated previously, however, those who do not have such sensations could still have immediate, positive results. It is important to instruct patients to move their affected limbs actively and passively, if possible. Select either the Chorea and Tremor Area or the Foot Motor and Sensory Area, depending whether the patient has muscular spasms or other abnormal sensations such as pain or burning. Retain the needles for 30–45 minutes. Treatment is given two to three times per week and a therapeutic course consists of 10 treatments.
Scalp Acupuncture Points Pdf Online
RESULTS OF CASE #10
Barbara had very positive responses to scalp acupuncture treatment. As soon as we inserted two needles in her scalp at the Chorea and Tremor Area, the tightness in all four limbs loosened up and the spasms were gone. Soon after that, both of her arms began to move and lift. When we told Barbara that some similar patients were able to walk again, her eyes filled with tears. After inserting four more needles in her scalp, we encouraged Barbara to stand up. She was very surprised to find that she had regained the ability to control her legs again. Although she felt nervous and was assisted by two people, she stood up. She couldn't believe it when we encouraged her to start walking. With much excitement and audience applause, she followed our instruction and started to move: one step, then two, three, and four steps. She walked as much as she could, turning about every 30 steps, walking with confidence and a smile on her face.
At another scalp acupuncture seminar in Phoenix, Arizona, later the same year, the audience was waiting to see Barbara, whom we had treated several months before. We were astonished and barely able to recognize her when she walked into the conference room by herself. Barbara reported that she had not received further acupuncture treatment after the last two scalp acupuncture treatments because neither her insurance nor her own money could cover further sessions. Instead, she did intensive exercise as we had instructed seven months before and had recovered completely.
For the benefit of the seminar audience, Barbara demonstrated many different kinds of movement of her four extremities such as jumping, running, and easily raising her arms, which brought audience applause. She had gotten married and returned to work.
The only remaining problem was urgent, frequent urination and some incontinence of urine. That was one of the reasons that she returned to this second seminar half a year later. We put two needles in the Foot Motor and Sensory Area and two needles in the Reproductive Area. Barbara had constantly felt pressure and a “strange feeling” there, but she left the seminar very happy. She no longer had that urgent feeling in her bladder and was able to hold her urine for two hours.
DISCUSSION
We need to emphasize that this patient received only three scalp acupuncture treatments and had recovered completely. That is highly unusual and by no means the norm. Treating quadriplegia by acupuncture is very challenging. Normally it takes several months or even as much as one to two years for this treatment to be effective. Even then, only 50% of patients have a chance of improving. Quadriplegia can be treated after any duration, but less than three months from the date of injury or illness shows the greatest improvement. The longer the duration of impairment, the more gradual the improvement occurs. With long-term conditions expectations need to be realistic, although some patients will occasionally surprise practitioners.
There are many different acupuncture techniques to treat paralysis. Although scalp acupuncture has the best and fastest response, other techniques are necessary for a more complete recovery. Regular body acupuncture treatment has been found to have a positive therapeutic effect on the recovery of movement of hands, fingers, feet, and toes. Electrical stimulation is very helpful if the practitioner has difficulty rotating the needle more than 200 times per minute. Only two of the scalp needles should be stimulated at any one session, or the brain can become too confused to respond. For electrical stimulation in body acupuncture, fewer than four needles should be stimulated in each limb. The best results are usually achieved by applying low frequency (for example, 3 hertz) with high intensity (for instance, when visible muscle contraction is observed). Electrical stimulation can be applied above and below the damaged level at Hua Tuo Jia Ji points on the back, which is another important technique for treating quadriplegia in addition to scalp acupuncture.
Footnotes
a Editor's note: The references in this article have been renumbered for continuity.
b Publisher's note: We are choosing to use the authors' translation for the xian mai (). In A Practical Dictionary of Chinese Medicine, Wiseman and Feng translate this pulse image as the “string-like” pulse, but “wiry” is the more common usage.
REFERENCES
- >
- >
- >
- >
A Proposed Standard International Acupuncture Nomenclature: Report of a WHO Scientific Group
(1991; 36 pages)
Yamamoto New Scalp Acupuncture
| |||||||||||||||||||||||||||||||||
3.6 Scalp acupuncture lines
The Scientific Group considered the scalp acupuncture lines (Fig. 1-5) as well as the underlying functional zones of the brain (Fig. 6-7). It proposed the following nomenclature, using the alphabetic code MS (derived from “micro-system” and “scalp point”).
English name and location | Pinyin name | Han character name | Alphanumeric |
middle line of forehead 1 cun from GV24 straight down along the meridian | ézhongxiàn | MS1 | |
lateral line 1 of forehead 1 cun from BL3 straight down along the meridian | épángxiàn I | MS2 | |
lateral line 2 of forehead 1 cun from GB15 straight down along the meridian | épángxiàn II | MS3 | |
lateral line 3 of forehead 1 cun from the point 0.75 cun medial to ST8 straight down | épángxiàn III | MS4 | |
middle line of vertex from GV20 to GV21 along the midline of head | dingzhongxiàn | MS5 | |
anterior oblique line of vertex-temporal from qiánshéncong (one of the four acupuncture points collectively designated as Ex-HN1, 1 cun anterior to GV20) obliquely to GB6 | dingniè qiánxiéxiàn | MS6 | |
posterior oblique line of vertex-temporal from GV20 obliquely to GB7 | dingniè hòuxiéxiàn | MS7 Hi,Thank you for posting your query in Microsoft Community Forums.I understand that you are unable to hear any sound while using the Ableton live 9 lite application. Ableton. | |
lateral line 1 of vertex 1.5 cun lateral to middle line of vertex, 1.5 cun from BL6 backward along the meridian | dingpángxiàn I | MS8 | |
lateral line 2 of vertex 2.25 cun lateral to middle line of vertex, 1.5 cun from GB17 backward along the meridian | dingpángxiàn II | MS9 | |
anterior temporal line from GB4 to GB6 | nièqiánxiàn | MS10 | |
posterior temporal line from GB8 to GB7 | nièhòuxiàn | MS11 | |
upper-middle line of occiput from GV18 to GV17 | zhenshàng zhèngzhongxiàn | MS12 | |
upper-lateral line of occiput 0.5 cun lateral and parallel to upper-middle line of occiput | zhenshàng pángxiàn | MS13 | |
lower-lateral line of occiput 2 cun from BL9 straight down | zhenxià pángxiàn | MS14 |
Scalp Acupuncture Points Pdf
Fig. 1. Scalp acupuncture lines MS1, MS2, MS3 and MS4 (anterior view)
Fig. 2. Scalp acupuncture line MS5 (vertex view)
Scalp Acupuncture Map
Fig. 3. Scalp acupuncture lines MS6 and MS7 (lateral view)
Fig. 4. Scalp acupuncture lines MS8, MS9, MS10 and MS11 (lateral view)
Fig. 5. Scalp acupuncture lines MS12, MS13 and MS14 (posterior view)
Fig. 6. Scalp acupuncture lines MS6, MS7, MS8, MS9, MS10 and MS11 superimposed on functional zones of the brain*
* These scalp acupuncture lines were formerly named in functional terms. The proposed standard international nomenclature is based on surface anatomy so as to facilitate localization of the lines, but their relationship to the underlying functional structures has not changed.
Fig. 7. Scalp acupuncture lines MS12, MS13 and MS14 superimposed on functional zones of the brain*
* These scalp acupuncture lines were formerly named in functional terms. The proposed standard international nomenclature is based on surface anatomy so as to facilitate localization of the lines, but their relationship to the underlying functional structures has not changed.